Coronary Artery Bypass Surgery
CABG is a surgical procedure in which one or more blocked coronary arteries are bypassed by a blood vessel graft to restore normal blood flow to the heart. These grafts usually come from the patient’s own arteries and veins located in the chest (thoracic), leg (saphenous) or arm (radial). The graft goes around the blocked artery (or arteries) to create new pathways for oxygen-rich blood to flow to the heart.
The goals of the procedure are to relieve symptoms of coronary artery disease (including angina), enable the patient to resume a normal lifestyle and lower the risk of a heart attack or other heart problems.
At CIMS Hospital, bypass surgery may be performed in combination with other heart surgeries, when necessary, such as valve surgery, aortic aneurysm surgery or surgery to treat atrial fibrillation (an irregular heart beat)
Who is eligible to receive coronary artery bypass graft surgery?
Diagnostic tests have helped your heart doctor identify the location, type and extent of your coronary artery disease. The results of these tests, the structure of your heart, your age, the severity of your symptoms, the presence of other medical conditions, and your lifestyle will help your cardiologist, surgeon and you determine what type of treatment is best.
At CIMS Hospital, CABG surgery may be combined with other heart surgeries, such as valve surgery, aortic aneurysm surgery or surgery to treat atrial fibrillation (an irregular heartbeat).
What happens during the cardiac bypass surgery?
After general anesthesia is administered, the surgeon removes the veins or prepares the arteries for grafting.
There are several types of bypass grafts. The surgeon decides which graft(s) to use, depending on the location of the blockage, the amount of the blockage and the size of the coronary arteries.
Graft used for bypass
- Internal mammary arteries [also called IMA grafts or internal thoracic arteries (ITA)] are the most common bypass grafts used, as they have shown the long-term results. In most cases, these arteries can be kept intact at their origin because they have their own oxygen-rich blood supply, and then sewn to the coronary artery below the site of the blockage. If the surgeon removes the mammary artery from its origin, it is called a “free” mammary artery. Over the last decade, more than 90% of all patients received at least one internal artery graft. At CIMS Hospital we use more of this conduits as it gives good long term results.
- The radial (arm) artery is another common type of arterial graft. There are two arteries in the arm, the ulnar and radial arteries. Most people receive blood to their arm from the ulnar artery and will not have any side effects if the radial artery is used. Careful preoperative and intraoperative test determine if the radial artery can be used. If the radial artery is used as the graft, the patient may be required to take a calcium channel blocker medication for several months after surgery. This medication helps keep the artery open. Some people report numbness in the wrist after surgery. However, long-term sensory loss or numbness is uncommon.
- Saphenous veins can be used as bypass grafts. Minimally invasive saphenous vein removal does not require a long incision. One to two incisions are made at the knee and a small incision is made at the groin. This results in less scarring and a faster recovery. Your surgeon will decide if this method cardiac bypass surgery is a good option for you.
What are the risks?
As with any surgery, there are risks involved. Your surgical risks are related to your age, the presence of other medical conditions and the number of procedures you undergo during a single operation. Your cardiologist will discuss these risks with you before surgery; please ask questions to make sure you understand why the procedure is recommended and what all of the potential risks are.
Surgical Procedure
To bypass the blockage, the surgeon makes a small opening just below the blockage in the diseased coronary artery. If a saphenous (leg) or radial (arm) vein is used, one end is connected to the coronary artery and the other to the aorta. If a mammary artery is used, one end is connected to the coronary artery while the other remains attached to the aorta. The graft is sewn into the opening, redirecting the blood flow around this blockage.
The procedure is repeated until all affected coronary arteries are treated. It is common for three or four coronary arteries to be bypassed during surgery.
Before the patient leaves the hospital, the doctor or nurse will explain the specific bypass procedure that was performed.
Heart-Lung Machine
During surgery, the heart-lung bypass machine (called “on-pump” surgery) is used to take over for the heart and lungs, allowing the circulation of blood throughout the rest of the body. The heart’s beating is stopped so the surgeon can perform the bypass procedure on a “still” heart.
Off-pump or beating heart bypass surgery allows surgeons to perform surgery on the heart while it is still beating. The heart-lung machine is not used. The surgeon uses advanced operating equipment to stabilize (hold) portions of the heart and bypass the blocked artery in a highly controlled operative environment. Meanwhile, the rest of the heart keeps pumping and circulating blood to the body.
Minimally Invasive Technique
Minimally invasive coronary artery bypass (MIDCAB) surgery is an option for some patients who require a left internal mammary artery (LIMA) bypass graft to the left anterior descending (LAD) artery.
Other minimally invasive surgery techniques include endoscopic or keyhole approaches (also called port access, thoracoscopic or video-assisted surgery) and robotic-assisted surgery. The benefits of minimally invasive surgery include a smaller incision (3 to 4 inches instead of the 6- to 8-inch incision with traditional surgery) and smaller scars. Other possible benefits may include a reduced risk of infection, less bleeding, less pain and trauma, decreased length of stay in the hospital (3 to 5 days) and decreased recovery time.
The surgical team will carefully compare the advantages and disadvantages of minimally invasive CABG surgery versus traditional CABG surgery. Your surgeon will review the results of your diagnostic tests before your surgery to determine if you are a candidate for any of these minimally invasive techniques.
How long does the procedure last?
The surgery generally lasts from 3 to 5 hours, depending on the number of arteries being bypassed.
Pre Surgery
You will be admitted one or two days prior to the operation. Sometimes, the surgery can be performed on the same day of admission. In either case, following is the pre operative protocol performed on all patients.
- A blood and urine test will be done to ascertain that everything is in proper balance and to ascertain baseline values.
- A chest X-ray and an electrocardiogram will be taken.
- A lung function test will be done.
- A solution will be given for oral care.
- The anesthesiologist will meet you before surgery and pre-operative medications for the day of the surgery. This medication causes drowsiness, but you will not be completely sedated at this time.
- The physiotherapist (your case co-ordinator) will visit and explain about exercise to be performed during and after hospitalization.
A member of the surgical team, will visit the patient and family to explain what the surgery is all about and what will happen in the Intensive Care Unit (ICU) when one awakes after surgery. It is strongly advised that the patient visit the ICU before surgery, he does not find himself in an unknown area.
The Day of the Surgery
An hour before you wheeled into the operation theater, you will be called into the ICU & will receive a preoperative antibiotic injection to prevent infection and an injection which will help you relax and make a little drowsy.
- Once wheeled into the operating room, one will not be put to sleep i.e. anesthized for about 15-20 minutes.
- The anesthesiologist will prepare you by putting in several lines. Certain discomfort may be experienced, while the lines are being inserted.
- One or two lines are inserted in one of the arms.
- An arterial line is inserted into the artery of the wrist to monitor blood pressure.
- Another line, Swan Ganz catheter or Triple lumen catheter will be inserted into large vein in the neck after anaesthetisation which monitors the heart pressures during the operation.
- Once all lines are inserted, you will be anesthetized through medication given into the IV lines.
- After anaesthesia, a breathing tube is inserted through mouth or nose, and the operation begins.
A member of the surgical team, will visit the patient and family to explain what the surgery is all about and what will happen in the Intensive Care Unit (ICU) when one awakes after surgery. It is strongly advised that the patient visit the ICU before surgery, he does not find himself in an unknown area.
After Surgery
In the Intensive Care Unit:
You will be brought directly to the ICU from the operation theater. You will feel drowsy and be sedated for 4-6 hrs after the operation due to effects of anesthesia. The breathing will be mechanically assisted by a ventilator with oxygen going in through the tube. Normally, one person of the family can visit the patient in the ICU one to two hours after the operation.
Many tubes will be attached to the patients body soon after the operation such as:.
- Nasogastric tube (Stomach tube): It will be put in the nose, going down into the stomach to prevent gastric distention and nausea. This tube causes no pain but may cause some post-nasal drip. The tube may be removed the next morning.
- Breathing (endotracheal or E.T) tube: Connected to a ventilator or (breathing machine) the purpose is to ensure deep breaths and make it easier to breathe.
- When you awaken, you will not be able to talk because the breathing tube goes down between the vocal cords.
- You will be able to communicate by writing notes or nodding your head.
- Hands may be gently restrained to remind you not to pull tube out.
- Suctioning of the breathing tube will be done, as needed, to remove secretions and prevent pulmonary problems.
- A coughing sensation may be experienced when the breathing tube is suctioned.
- The tube will be removed as soon as you are awake and breathing adequately on your own.
- Once tube is removed, your throat may be sore and you may be hoarse.
- When you cough out sputum, it may be blood tinged due to irritation from the tube. All of these conditions are temporary and normal.
- Foley catheter: It will be inserted into your bladder while you are asleep to accurately measure and record urine output. You may still feel the urge to urinate even with the catheter.It will be removed on the 2nd postoperative day. There may be a burning sensation the first time you urinate after the Foley catheter is removed.
- One or two tubes will be inserted in your chest at the end of the operation. The purpose of the chest tube(s) is to prevent accumulation of fluid in the chest cavity. Chest tube(s) will be gently squeezed or milked to ensure adequate drainage. When the family comes in to visit they will see drainage container at the foot of the bed with some bloody drainage in it. This is entirely normal. The chest tube(s) will be removed when some bloody drainage in it. This is entirely normal. The chest tube(s) will be removed when the drainage stops, usually on the second day.
- An arterial line is a soft plastic needle that is inserted into the radial artery in the wrist to monitor the blood pressure. For the first day any blood sample that are necessary for tests can be drawn from the arterial line. It is usually removed on the first postoperative day.
- IV lines will give you fluid, medications, and blood when needed. The IVs are removed the morning after surgery.
First Day After Surgery
- When you are awaken, you will be taken off the ventilator and allowed to breath on your own. The breathing mask, which supplies humidified oxygen, will still be in place on your face.
- The nasogastric tube will be removed.
- You will be taught how to perform coughing and deep breathing exercise.It may seem uncomfortable but is beneficial and will not cause any damage to the heart, grafts or incisions.
- You will be turned from side to side at least every four hours to relieve pressure areas.
- Clear liquids will be given several hours after the breathing tubes have been removed and then there will be a gradual process to a regular diet.
- If the condition is stable, some of the monitoring lines will be removed. The only line left will be an IV or heparin lock.
- The chest tube(s) remains in place for 4-5days.
Second Day After Surgery
Depending on the medical condition, the following protocol will be observed on the second day.
- Once the patient acquires an appetite, he can begin to eat regular food, but the fluid intake will be limited to 6 cups (48oz.) to 8 cups (64oz.) in 24 hours.
- One of the chest tube(s) will be removed. Pain medication will be given prior to this procedure.
- You may have one or two tubes attached to a bag which can be carried.
- Foley catheter will be removed on the 2nd day after surgery.
- Chest physical therapy will begin as indicated.
- After the chest tube(s) have been removed, you will be assisted out of bed and into the chair.
- One may experience tiredness and fatigue as a result of stay in the ICU. Depression and discomfort is common. But it is important to let the nurse know so that she/he can administer pain medication. If the comfort level is satisfactory it will be easier to do breathing and coughing exercise and to get out of bed and walk.
- You will be shifted to room/ward after 2-3 days depending upon surgery & recovery.
Postoperative Discomfort and Expected Minor Complications
- Pain
It is natural to have aches and pains after surgery. Your physician will prescribe pain medication, which should be taken when needed. The nurses will ask you if you have pain in either chest or leg incision, but it is your responsibility to ask the nurse for pain medication. A good time to request the pain medication is 15-20 minutes before beginning your breathing exercises.
- Pericarditis
The pericardium is a thin lining (sac) around the heart that is opened during the surgery.
Normally, there is a small amount of fluid in the pericardial sac, and the heart moves easily within it.
The sac may become inflamed and irritated as a result of the surgery, and this will cause discomfort in the chest, shoulder and neck. The soreness can be mild to severe.
Sweating may occur especially at night. The discomfort can increase with deep breathing, coughing, or lying down.
It can be treated with one of several anti-inflammatory drugs or steroids. The discomfort subsides within a few days and the medication can be discontinued within a few weeks.
- Dysrhythmias
Dysrhythmias, or irregular heartbeats, can occur after surgery in 30% of patients & in particular old age patients. The patient may feel that his heart is racing, palpitating, or doing flip-flops.
There is no need to panic. Notify to nurse. An electrocardiogram may be done and, if necessary, medication will be started.
- Depression
This is a most common post-operative syndrome and can last for several days, or even months, after the operation. Sleep can be difficult in the ICU. There are noises, people and activity in the ICU 24 hours a day. You, may therefore feel tired, irritable, grumpy and even depressed. As one catches up on sleep after being shifted into the room, and the time of discharge approaches, the depression usually lessens or disappear.
- Coughing
After surgery, coughing and taking deep breaths might be painful, but coughing is extremely important.
Deep breathing is essential so that secretions do not build up in the lungs which could lead to a partial collapse of lungs, or even pneumonia. By coughing and deep breathing, secretions are discharged, thus keeping the lungs clear.
- Bleeding
Bleeding can occur after surgery. The drainage from the chest tube(s) is observed closely for any signs of excessive bleeding. Occasionally a patient is returned to the operating room for control of the bleeding. The procedure takes about an hour. The patient is returned to the ICU. This can occur in 20% of cases after the procedure is normal.
- Remaining days in the Hospital
The day you are transferred to the regular unit, you should walk in your room and sit in a chair two or three times.
The next day, you should walk in the hallway; at first, walk with assistance until you are more steady on your feet. Do lot of exercise & physiotherapy.
For the remainder of your hospital stay you should start walking more and more in the hallway. By the time you leave the hospital you may be able to walk up to one mile a day (not all at one time) and climb 7-8 steps. You may not feel like eating for a few days which is normal because of antibiotics & medicines.
You will probably be ready to leave the hospital 6 to 10 days after your surgery. The remainder of your recovery will take about four to eight weeks at home.
- From Hospital to Home
It is extremely normal to feel anxious or depressed about leaving the hospital which has provided you with a sense of security. Do not forget, that you will not be discharged until the doctors are confident of your fitness to go home.
Once home, try to resume a normal routine.
It is important to arise at a reasonable time, have a bath and dress in clean clothes.
This simple act will help you greatly in feeling normal and aid your recovery process.
It is available to discuss with your doctors the apprehensions you and your family feel.
The following points need to kept in mind while going home:
- Appointments for check ups. On the day of discharge, you should fix up an appointment with your heart surgeon/cardiologist for check-ups.
- The surgeon might want to see you 4 weeks post-discharge.
- Your cardiologist/family physician will be responsible after the surgeon has discharged you and the post-operative visits are over.
- You should contact the surgeon’s office, if any problems arise before the next appointment. Take appointments with your local doctor & family physicians after returning home.
Care & Concerns at Home
- Incision Care
The sutures (if any) on the chest or leg will be removed 7 days after discharge. After suture removal take regular bath twice a day with thorough cleaning of suture lines with soap and water.
The remaining stitches are self-absorbing and will absorb in about two months. Some redness, tenderness, swelling will be present for several months.
Inspect the incision(s) and notify the physician/surgeons in case of infection.
Increased redness, tenderness, swelling or a pus-like drainage from the incisions may indicate infection.
- Sexual Activity
The average demand on the heart during intercourse is equivalent to walking briskly for several minutes along with climbing two flights of stairs.
One can include in sexual activity after heart surgery. It is a common fear that one may experience difficulty in getting or maintaining an erection, lack of stamina or trouble having an orgasm.
Sexual activity can be resumed after the return visit to the surgeon. It should be indulged only after the partner is well rested, not eaten a heavy meal and is relaxed. One should be in a more passive position and not place weight on the arms for the first six weeks. The breastbone requires approximately 6-8 weeks to heal and strain should be avoided during this period.
- Memory and Vision Changes
You may find it difficult to remember things or to concentrate after surgery. Full functioning of memory and concentration abilities is achieved within a few weeks.
Vision change is common post operatively. This is due to use of the heart lung machine used during surgery. Do not rush to get glasses for vision correction.
These changes correct themselves within six months of the surgery. If vision or mental function change persists, one should notify the family physician.
- Climbing
One can climb stairs, but one has to do it slowly.
One should rest if one become tired, short of breath or dizzy. It is better to limit climbing stairs to two to three times a day for the first two weeks.
- Smoking
Smoking has to be completely stopped.
Smoking increases the heart rate, narrows the blood vessels, raises blood pressure and affects the lungs.
It is difficult to quit smoking but it is extremely important to do so.
- Rest Periods
The body needs more sleep during the healing period.
It is essential to get 8-10 hours of sleep at night. During the day, rest periods are essential. One should not indulge in activity for more than 2-3 hours. Resting after 2-3 hours of work is necessary to avoid strain.
It is not necessary to sleep during the rest periods, one can just relax.
Visitors at home should be limited, especially during the first two weeks at home.
- Recreation
Physical activities (tennis, swimming, bowling, golf) other than walking should be postponed for 10-12 weeks.
Physical activities which do not involve exertion can be indulged in such as playing cards, going out for dinner, movies or theatre, or social visits can be indulged in.
- Depression
It is extremely common to feel depressed after surgery.
However there is a difference. Being depressed is different from clinical depression which is a condition wherein a patient is depressed, but also is prone to other symptoms such as insomnia, appetite disturbances, fatigue, lethargy, lack of interest in pleasure-giving things including sexual intercourse and feelings of hopelessness and despair. Suicidal thought too can occur.
If such symptoms occur, the physician should be contracted so that treatment can be commenced.
- Constipation
If the patient is constipated after discharge, laxative can be taken.
Isabgol is best for constipation and should be taken daily at night time.
Increase the intake of fluids, green vegetable and fruits.
If discharged on an iron pill, the bowel movements will be black.
- Diet and beverages
One can drink coffee or tea but not more than two cups a day.
Cola drinks, chocolate, tea and some pain medications contain caffeine or caffeine-like substances- so include them in calculating the intake of two cups a day.
Stay away from non-dairy creamer and cream in coffee, as these contain considerable amounts of saturated fats. Try to use non-fat powered milk, 1% low fat milk, skim milk or evaporated milk. Black tea or coffee would be an ideal drinking choice. Initially after surgery, one may not have much of an appetite, which will improve over time.
It is important to maintain an adequate and nutritious diet after surgery to quicken the process of healing, and gaining strength and good health.
Iron is an essential for recuperation.
Too much fat and the wrong kind of fat can be harmful to the body. Saturated fat increases the level of cholesterol in the blood. Saturated fat is usually sold at room temperature and mostly found in most animal foods such as
- White of milk or 2% milk
- Butter & Cheese
- Meat
- Some vegetable products such as coconut and palm oil
- Chocolate
Some saturated fats can be made from unsaturated fats through a chemical process called hydrogenation which should be avoided.
polyunsaturated fats lower the level of cholesterol in the blood. These fats are from vegetable sources and some of them are:
(1) Sunflower oil (2) Soyabean oil (3) Sesame seed oil (4) Safflower oil (5) Cottonseed oil (6) Corn oil
The diet should be planned in consultation with the cardiologist/family physician.
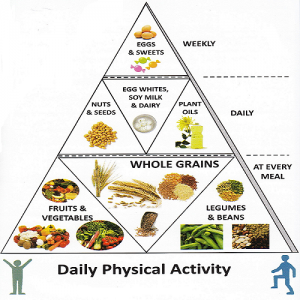
- Dietary guidelines in planning balanced diet :
- Patient should maintain slightly lower than the standard weight. Accordingly, total calories should be restricted.
- The diet should be rich in fiber including foods like raw salads, fruits, green leafy vegetables and whole grains.
- Five servings of fruits and vegetables should be included in the diet not only to meet the nutritional requirement but also to meet antioxidants and fibre.
- Consumption of two or more oils help in obtaining the optimal ratio of different fatty acids.
- Inclusion of fish in the diet is beneficial as they contain omega-3 fatty acids.
- Concentrated foods like sweets, chocolates, cakes, pastries, ice creams and fried foods should be restricted.
- Foods giving only empty calories like carbohydrated beverages, alcohol, sugar and sago are to be totally avoided.
- Small quantities of almond can be consumed to bring down the cholesterol levels. High amounts of nuts and oil seeds increase the calories and fat content in the diet.
- Coconut should be avoided in the diet as it contains high amount of saturated fatty acids and it is a concentrated source of energy.
- Coffee and tea can be taken in moderation. Excess amount of caffeine can increase the heart rate.
- Animal foods like meat and pork which contain high amount of saturated fat should be avoided. All sea foods are rich in sodium, hence hypertensive patients should avoid these foods.
- Foods that have hypercholesterolamic effects like soyabean, fenugreek, garlic, onion and turmeric should be included in the diet.
- Heavy meals should be avoided as they are mostly high in fat.
- Taking outside meals are to be avoided as they mostly are high in fat.
- Constipation should be prevented by including plenty of water and fibre in the diet.
- Best cooking oils:
- For deep frying foods: The best oils are those with a high smoke point such as canola oil, safflower oil and sunflower oil
- For stir frying and salad dressing: Any oil low in saturated fat like canola oil, corn oil, or flaxseed oil, olive oil, peanut oil, walnut oil, sunflower oil and safflower oil.
- Return to work
After the surgeon gives his consent after the 4-week check up, most patients can return to work in 6-10 weeks, depending on the occupation. After a one month follow-up with surgeon and the cardiologists opinion, one can resume work slowly with light duty initially.
- Balance Diet Chart
| Meal and time | Menu | Quantity |
|---|---|---|
| 6:00 to 7:00 a.m. | ||
| Tea/coffee/milk | 1 cup | |
| Marie biscuits / Khakhara | 2 / 1 | |
| Morning breakfast 9:00 to 10:00 a.m. |
Milk | 1 cup |
| Poha / Upma / Sprouted grams
OR |
1 katori | |
| Phulkas / Idly / Paratha OR | 2 / 2 / 1 | |
| Vegetable sandwich (w/o butter) | 2 slice | |
| One fruit | ||
| Lunch 12:00 to 1:00 p.m. |
Salad | 1 cup |
| Subji (green leafy or others) | 1 katori | |
| Roti / Chicken / Fish / Egg white | 2-3 / 50gm / 1 | |
| Dal / Kadhi | 1 Katori | |
| Rice | 1/2 Katori | |
| Curd / Buttermilk | 1/2 cup / 1 glass | |
| Evening 3:30 to 4:30 p.m. 5:00 to 6:00 p.m. |
Tea / Coffee / Lemon juice | 1 cup / 1 glass |
| Biscuits / Mumara / Roasted Poha | 2-3 / 1 Katori | |
| One fruit | ||
| Dinner 7:30 to 8:00 p.m. |
Roti | 2 small |
| Subji | 1 Katori | |
| Khichdi / Dalia | 1 Katori | |
| Bed time | Milk (low fat) | 1 glass |
Note:
- 2 to 3 almond, 1 walnut and 1 anjir/khajoor (dates) take daily.
- Take low fat milk.
- Use two or more oils separately.
- 1 cup = 150 ml, 1 glass = 200 ml, 1 katori = 200 gm.
CARDIAC SURGICAL
Together Everyone Achieves More
We are a team of cardiac thoracic & vascular surgeons and cardiac anaesthestists and intensivists providing world class surgical services in the heart of Ahmedabad. Totally committed to provide our best with no compromises on patient management and ethics.
Integrating experience and expertise of different world class centre at one place.
Values at Heart of our practice
- Clinical Excellence: To surpass toughest quality benchmark.
- Team Work: Leveraging group genius to patient’s advantage.
- Integrity: Upholding the faith reposed in us.
- Vision: To learn, share and explore new frontiers of Cardiac Surgery.
We excel in:
High risk open heart surgery: Especially CRF patients, COPD patients, old age/geriatric patients, multivalvular surgeries and surgeries in severe LV Dysfunction and Redo surgeries.
Heart failure surgery: It includes LV Volume Reduction surgeries like Dor’s procedure, SVR, geoform Functional Mitral Valve Repair.
Mitral Valve Repair: Trying to retain original valve tissue for better heart functioning & better quality of life.
Minimally invasive surgery: for various valve repairs/ replacements, selected cases of CABG and ASD Closure.
Pediatric Cardiac surgery: Simple and complex congenital cardiac procedures.
We routinely perform:
- Off-pump, On-pump CABG
- Total arterial CABG
- Aortic surgery
- Major Vascular surgery
- Thoracic surgery
- Post cardiac surgery rehabilitation
- Pain clinic
| Dr. Dhiren Shah MB, MS, MCh (C.V.T.S) (Cardiothoracic & Vascular Surgeon) Director, CIMS Hospital (M) +91 9825575933
|

